Turkana County in northwestern Kenya was supposed to be the land that malaria forgot. An arid, windy region abutting Uganda, South Sudan and Ethiopia, its climate was thought to be too dry for the mosquitoes that harbor malaria-causing parasites, and thus it has been excluded from national efforts to prevent the spread of the disease.
But that assumption may have been wrong, according to a new study by malaria researchers at the Duke Global Health Institute and Moi University in Kenya. And worse, it may leave an opening for new forms of malaria that could reverse the progress East Africa has made in controlling the disease.
“These findings are game-changers for malaria control in East Africa,” says Wendy Prudhomme O’Meara, Ph.D., a professor of medicine and global health at Duke who led the research.
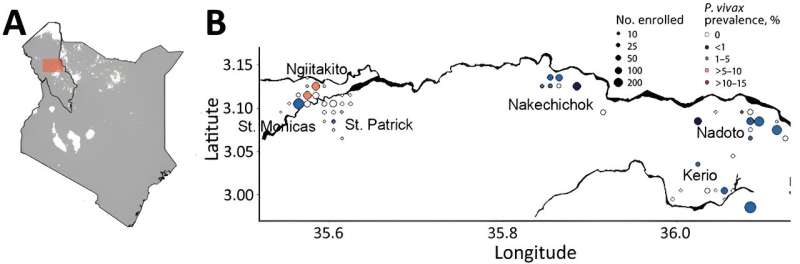
O’Meara’s team found that approximately 30 percent of the people they tested in Turkana County had malaria parasites in their blood, indicating that the disease was already endemic in the region. But even more concerning was the type of malaria: Researchers found a small but significant incidence of a parasite called Plasmodium vivax, which historically has been almost non-existent in sub-Saharan Africa. The study is the first to confirm cases of P. vivax malaria in Kenya that were likely the result of local transmission.
The parasite’s appearance in Kenya may be connected to an invasive mosquito species known as Anopheles stephensi, which migrated to the Horn of Africa during the past decade and has been found in five countries in northern Africa.
Its arrival in Djibouti in 2016 coincided with a 100-fold increase in malaria cases, leading the World Health Organization to issue an alert about the insect’s invasion, calling it “a major potential threat to malaria control and elimination” on the continent.
“If we don’t do something about it, we’re going to be in trouble very soon,” says Eric Ochomo, Ph.D., a medical entomologist with the Kenya Medical Research Institute who identified the invasive species in northern Kenya in December 2022, around the same time as O’Meara’s study.
Both the mosquito and the parasite it carries present significant challenges to the continent’s malaria control efforts, the researchers warn. P. vivax behaves differently than the most prevalent forms of malaria in Africa, which can allow it to evade screening tests and therapies most frequently used across the continent. It can go dormant in the liver, causing relapses weeks or months after infection.
“We are worried that with the presence of the An. stephensi, cases of P. vivax malaria may very well increase,” says O’Meara, who has been working on malaria prevention in Kenya since 2003. “There are no measures in place for P. vivax malaria control in Kenya, and it needs some targeted mechanisms.”
Native to India, Anopheles stephensi mosquitoes thrive around sewers and dirty water, making them more adaptable to urban areas. The fact that they are breeding successfully in hot, dry regions like Turkana should cause public health officials to rethink their assumptions about malarial hot spots, Ochomo says.
“Areas that are either approaching elimination or that are categorized as low risk are going to end up with higher prevalence than they currently see,” he says.
O’Meara’s team shared their findings with Kenya’s National Malaria Control Program, which is now ramping up distribution of mosquito nets and surveillance in Turkana County. The researchers also plan to work with community members to identify and eliminate potential mosquito breeding grounds.
A spike in P. vivax cases could also undermine what was thought to be a genetic firewall against the parasite spreading on the continent. Many Africans have a genetic trait that is believed to protect against P. vivax infection, which is one reason cases have been relatively rare. But O’Meara says there are signs that recent outbreaks may be affecting even those with the genetic protection, a reminder that the parasite is constantly evolving new ways to evade defenses.
“The malaria parasite has successfully transmitted between humans and mosquitoes for tens of thousands of years,” she says. “The co-evolution of the parasite with humans has made it incredibly difficult to eliminate.”
More information:
Wendy Prudhomme O’Meara et al, Plasmodium vivax Prevalence in Semiarid Region of Northern Kenya, 2019, Emerging Infectious Diseases (2023). DOI: 10.3201/eid2911.230299. wwwnc.cdc.gov/eid/article/29/11/23-0299_article
Citation:
Endemic malaria found in high, dry northwestern Kenya (2023, October 12)
retrieved 12 October 2023
from https://medicalxpress.com/news/2023-10-endemic-malaria-high-dry-northwestern.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.