While reading the Summer 2023 issue of the University of Michigan Medical School alumni magazine, I came across a delightful article on Dr. Hannah Abraham, who had just received her MD and PhD degrees from Michigan. The article included a photograph of her receiving her diploma from Dr. Robert Bartlett, professor emeritus of surgery.
According to the article, Hannah was born with her umbilical cord wrapped around her neck and was close to dying by asphyxiation. She was airlifted to Michigan’s C.S. Mott Children’s Hospital, where Dr. Bartlett and his care team were able to save her life with a special device called extracorporeal membrane oxygenation (ECMO). Years later, Hannah enrolled at University of Michigan for college and medical school. This summer, she was presented with her diploma by Dr. Bartlett.
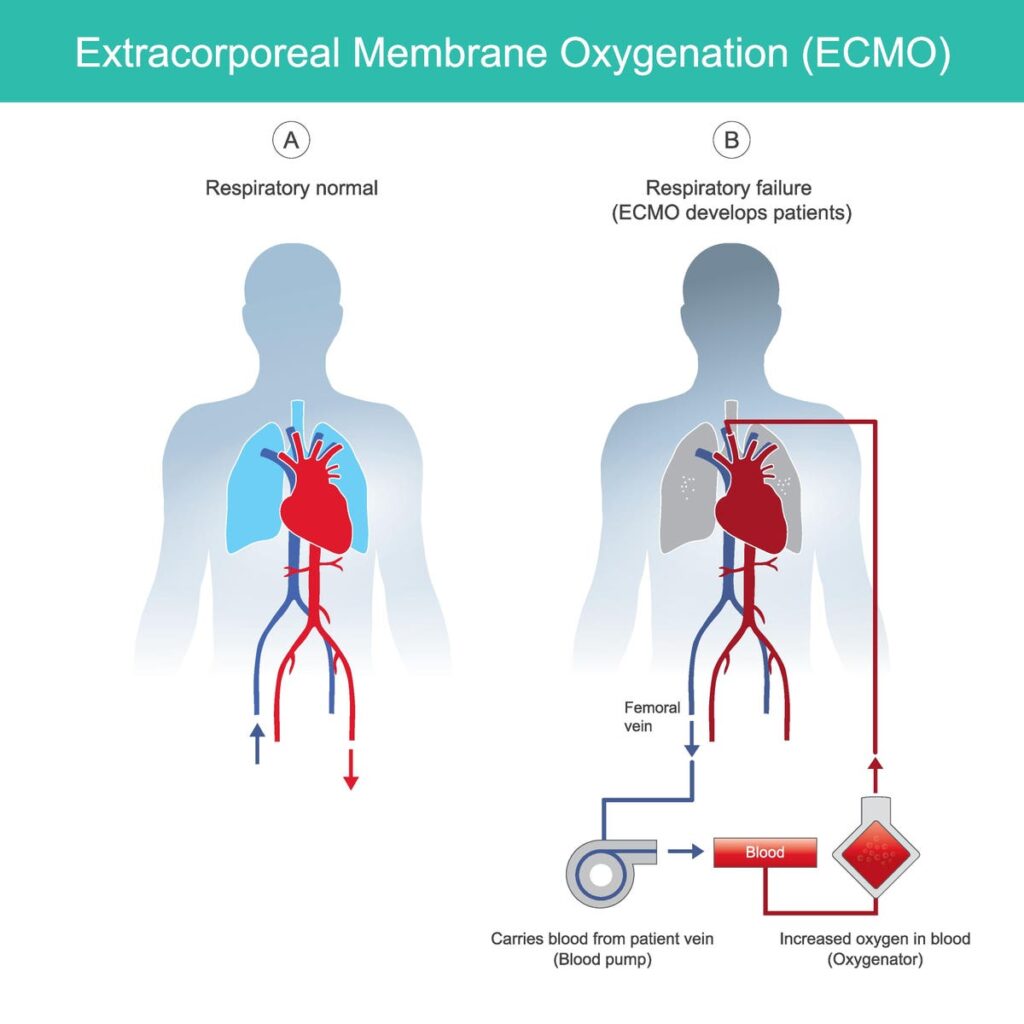
Extracorporeal membrane oxygenation. diagram for explain rescue patients respiratory failure by … [+]
Dr. Bartlett himself graduated from University of Michigan Medical school in 1963, and was later Professor of Surgery at Michigan. He is often called the “Father of ECMO” for his development of this life-saving technology.
In patients with badly damaged lungs, the lungs can no longer transport oxygen from the air into the blood stream (or transport carbon dioxide from the blood back into the air).
The ECMO system takes the patient’s blood and passes it through an “artificial lung” which consists of specially designed membranes that allow safe contact between the blood and oxygen gas. The artificial lung pushes fresh oxygen into the blood (and pulls carbon dioxide out of the blood), then returns the oxygen-replenished blood to the patient’s body.
Early in his surgical career, Dr. Bartlett thought the ECMO idea could work. According to Bartlett, “most neonatologists thought this was a pretty crazy, far-fetched project.” But he persisted in his research.
In 1976, Dr. Bartlett reported the first use of ECMO to save the life of an infant whose lungs were badly damaged during the birth process from inhaling amniotic fluid contaminated with fetal stool. This was considered a last-ditch treatment. After 3 days on the ECMO machine, the infant recovered.
Since that time, ECMO has been used in numerous pediatric and adult patients suffering from a variety of serious lung and heart conditions.
During the Covid-19 pandemic, many patients suffered such severe lung damage that normal “breathing machines” (ventilators) were insufficient to help them. Those who were able to receive ECMO therapy showed a 45% reduction in mortality compared to those who did not receive ECMO.
ECMO has saved thousands of lives over the years across the world, including Dr. Abraham’s. I’m delighted she was able to receive her degree, and I wish her much success and happiness in her future medical career.
(Personal note: When I was a third-year medical student at Michigan on the trauma surgery rotation, I had the honor of “scrubbing in” with Dr. Bartlett on several cases. I remember him as a highly skilled surgeon with a kind and compassionate bedside manner. I feel fortunate to have been able to work with a legend of American surgery.)