The United States Preventive Services Task Force on Tuesday created new draft guidelines recommending all women begin screening mammography at age 40, a decade earlier than previous guidelines, and continue screenings every other year until age 74.
The change is bound to be controversial, adding fresh fuel to a long-standing debate around when people should begin breast cancer screening, how often they should do it, and if specific groups, such as Black women, ought to be screened differently.
The task force is widely considered to be the most influential voice in population health recommendations, and some of its recommendations determine what procedures health insurers must cover. But its latest decision has seemed to please few cancer screening researchers, with some saying the new guidelines overstep while others argue they don’t go far enough.
Independent experts say they’re also unsure why the task force chose to update the guidelines now, given that the statistical models that help guide the screening have not shown dramatically different results since the panel’s last mammography guidelines in 2016.
“I think people are going to be surprised,” said Ruth Etzioni, a biostatistician who studies cancer screening at the Fred Hutchinson Cancer Center and who is not a task force member. “Change always happens over time, obviously, as the evidence evolves. At the same time, there needs to be a compelling reason and in the materials here, I don’t see a compelling reason yet.” She added: “When I looked back at the 2016 modeling studies, the harm-benefit analysis was very similar.”
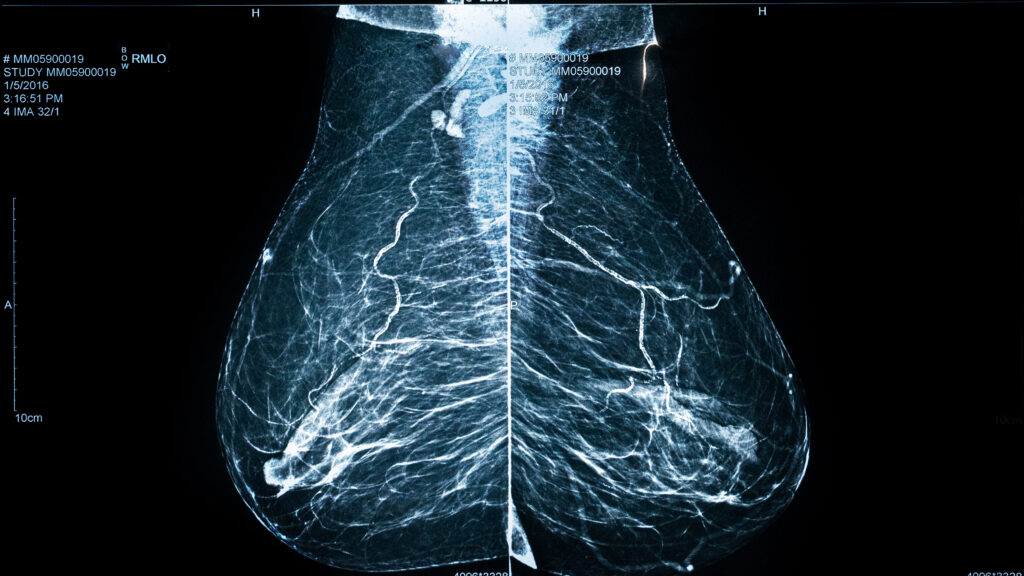
All cancer screening, including mammography, has the same goal: catch cancers earlier when they’re easier to treat and, often, still curable with procedures like surgery, radiation, and chemotherapy. But this also means screening millions of people before they have any sign of disease — which would be an easy policy to espouse if it was entirely harmless.
Breast cancer screening can save lives, and it has done so for countless individuals. But it can also lead to false positives, unnecessary biopsies, and — to a lesser degree — diagnosis or treatment of cancers that paradoxically never needed intervention.
Organizations that set screening guidelines, including the Preventive Services Task Force and the American Cancer Society, try to take into account both the benefits of saving lives and the potential harms of unnecessary screening. These organizations use the best available evidence from clinical trials, models, and incidence, morbidity, and mortality data to come up with their recommendations. How they settle on their recommended strategies while looking at the same data is “very much a judgment, as opposed to a clear scientific answer,” Etzioni said.
The American College of Radiology, for example, recommends starting breast cancer screening at age 40 and continuing every year. The task force, on the other hand, had recommended in 2016 that people start screenings at age 50 and go every other year until age 74, with people making individual decisions with their doctor about whether to get screenings in their 40s.
The American Cancer Society has a more moderate approach, recommending women start screening every year at age 45, with the option to switch to every other year at age 55.
Task force members say there were three main new pieces of evidence that played a role in creating new guidelines, which are now open to public comment.
The first is that recent data from the National Cancer Institute and the Breast Cancer Surveillance Consortium showed the breast cancer incidence among women in their 40s is steadily ticking up in women by a rate of 2% per year. “It’s more than we’ve ever seen before,” said John Wong, a task force member and an internist at Tufts Medical Center.
The second factor was an update in modern breast cancer screening technology, which can offer a slight reduction in false positives and an improvement in cancer detection, as well as updates on new, more advanced breast cancer treatments such as new targeted therapies, immunotherapies, and combination therapies.
Finally, Wong said, the task force also incorporated a new model that specifically analyzed the harms and benefits of different screening strategies for Black women. “We know African American women in general tend to have cancers diagnosed at later stages and subtypes that can be more aggressive, so this recommendation is particularly relevant for Black women,” said Wanda Nicholson, a task force member and an OB-GYN and epidemiologist at the George Washington University Milken Institute School of Public Health.
The task force updated its models with these new data and then compared the harms and benefits of screening every other year from age 50 to 74 to starting screening at 40 or 45 with the same intervals. Overall, the additional harms incurred from moving the starting age at 50 to 40, as measured by unnecessary biopsies and false positives, appeared to be slightly less in 2023 compared to what the models showed in 2016. But, the task force members said, the benefits now appear much greater.
“With this recommendation, we can see 20% more lives saved,” Nicholson said.
The models also showed that starting screening earlier led to a near doubling in life years gained, according to the task force’s Wong, compared to what the 2016 models had shown. Put another way, earlier screenings gave people more benefits for the same amount of harm by moving the age from 50 to 40 in the new models compared to the older ones in 2016. The benefits of earlier screenings were also much greater for specifically Black women, the task force said. Thus, the panel felt it was reasonable to recommend people begin screening at age 40.
That decision has rattled scientists from all sides of the cancer screening debate. “You’re kidding,” said Rita Redberg, the editor-in-chief of JAMA Internal Medicine and a cardiologist at the University of California, San Francisco, when she heard the new guidelines. “It is concerning to see a lowering of the age to start mammography,” she said, arguing that the panel failed to show the benefits of screening beginning at age 40 “will outweigh the harms of the practice.”
Other clinicians also reacted to the new guidelines with frustration, but for a different reason. “So, they definitely recommend starting at age 40, and the rest is every other year. That part should have changed, and it didn’t,” said Maxine Jochelson, the chief of the breast imaging service at Memorial Sloan Kettering Cancer Center and who is not on the task force.
Extremely aggressive cancers, like triple-negative breast cancer, can metastasize or spread within a couple years without clear symptoms. Recommending screening more frequently, Jochelson said, would help catch those cancers and give these people a better chance at survival. “Those are real women, and if you wait, they will present with metastatic disease.”
The task force also made a few other statements, noting that there was insufficient evidence to recommend a separate screening guideline for people with dense breasts, which can make it harder to detect lesions on mammograms, or for Black people. The guidelines also don’t apply to individuals with especially high risk for breast cancer, like those who are BRCA 1 or 2 gene carriers.
Those notes underscored the need for every person to think carefully about their personal preferences and risks for cancer, the task force’s Wong said. The guidelines, he said, are just that — recommendations.
“There’s always room for an individual woman to have a conversation with their trusted health provider with regard to mammography,” he said. Ultimately, how and when to screen should be an informed, but personal, decision.
This story has been updated.