A panel of experts that advises the Centers for Disease Control and Prevention on vaccinations opted Wednesday not to recommend that all seniors get a vaccine to protect against RSV.
Instead, the Advisory Committee on Immunization Practices said that anyone 60 and older should be able to get one of the new vaccines — being brought to market by GSK and Pfizer — if they and their physicians think it would be worthwhile.
Earlier in the day the committee looked set to vote on a stronger recommendation, one that would have urged all people 65 and older to get vaccinated against respiratory syncytial virus. But that recommendation was watered down after a long discussion during which several members of the committee expressed serious concerns about the decisions they were being asked to make based on the data the companies had provided.
In the end, the committee voted 9 – 5 to recommend that people 65 and older “may” get an RSV vaccine, based on shared decision-making, a term that typically means a discussion between patients and their doctors. With these vaccines, it could also mean a discussion between patients and their pharmacists, because the RSV vaccines will be covered by Medicare Part D and as such will be administered in pharmacies in most cases. (It is difficult for physicians to get compensated for administering vaccines covered by Medicare Part D.)
The committee voted 13 to zero, with one abstention, to recommend the same policy apply to people aged 60 to 64.
The recommendations now go to CDC Director Rochelle Walensky for her endorsement. Walensky is expected to sign off on the recommendations sometime late this week or early next.
The recommendations will likely lead to a lower uptake of the new vaccines than the manufacturers might have expected had the ACIP voted to accept the stronger “should” recommendation. At a point this spring, a GSK executive projected that sales of the RSV vaccine could rival those of Shingrix, the company’s very profitable shingles vaccine.
Both vaccines were approved for use in people aged 60 and older by the Food and Drug Administration last month. But the ACIP’s RSV adult vaccine working group has been indicating for some time that it did not see a cost-effectiveness argument for recommending that everyone between the ages of 60 and 64 get vaccinated against RSV.
GSK’s vaccine showed an overall vaccine efficacy of 82.6% against RSV-triggered lower respiratory tract illness in the first year after vaccination and 77.3% mid-way through the second year after vaccination. Pfizer’s vaccine showed an efficacy of nearly 89% against RSV lower respiratory tract infection involving at least three symptoms in the first year after vaccination, and 78.6% efficacy mid-way through a second RSV season.
Michael Melgar, a CDC epidemiologist who co-chairs ACIP’s RSV adult vaccine work group cautioned against comparing the two vaccines because the design of the clinical trials differed and the two companies were not measuring the exact same results.
The fact that the vaccines seem to protect for at least two years was new information presented at Wednesday’s meeting and was credited for a big jump in the estimated price of the GSK vaccine. Prior to this meeting, GSK had been talking about a per dose cost of around $148. On Wednesday, the committee learned during a presentation of an economic analysis conducted by the CDC and the University of Michigan that the GSK price estimate had jumped to $270.
Both companies resisted strong pressure from the committee to commit to a firm price, with ACIP members arguing they weren’t able to assess the cost-effectiveness of the vaccines without that information.
“None of us buy a car unless we know how much it costs,” said Helen “Keipp” Talbot, a geriatric infectious diseases specialist from Vanderbilt University. She urged the manufacturers to disclose their prices before the committee held its late afternoon vote. Just before the vote, the manufacturers came back with numbers, but both named a range.
Leonard Friedland, GSK’s vice president for scientific affairs and public health, said the company’s vaccine, which will be sold under the name Arexvy, will be priced within a “narrowed range” of between $200 and $295. Friedland argued that the cost reflects the fact that the vaccine’s coverage will last at least two years. A Pfizer executive told the committee the company is “in the middle of competitive price negotiations” and cannot give a firm cost figure for its vaccine. But she said the Pfizer vaccine, which will go by the brand name Abrysvo, would cost between $180 and $270.
It is expected both companies will provide vaccines to the market in time for the next RSV season, which is normally in the winter. Since the Covid-19 pandemic, however, RSV activity has begun in the late summer and early fall and it is unclear if and when the old pattern of activity will resume.
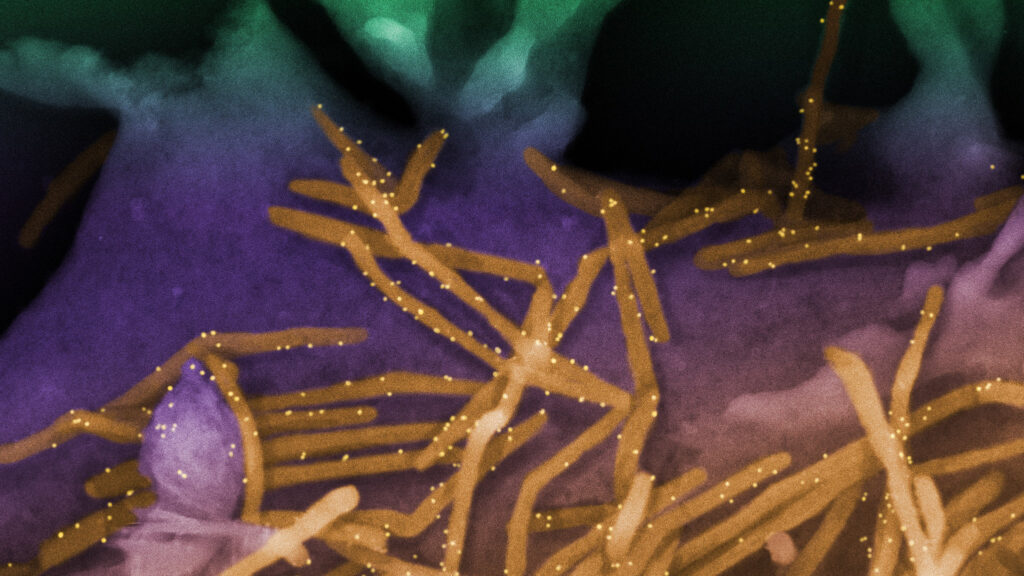
These are the first vaccines to protect against this virus, which is a significant cause of hospitalization among very young children and seniors. In older children and adults RSV infections typically manifest as colds.
While researchers who study RSV in adults have hailed the arrival of these vaccines, the experts on the ACIP have been frustrated by the data the companies presented.
Among their concerns was the fact that the clinical trials GSK and Pfizer conducted enrolled few adults 80 and older — the age group at highest risk from RSV. People who are immunocompromised and those living in congregate living settings such as nursing homes are also at elevated risk but were not enrolled in the studies.
Talbot noted that the committee is being asked to infer that because the vaccines were efficacious in the trials — largely in people in their 60s — they will also protect people in these other more vulnerable groups.
“Randomized controlled trials are needed to determine vaccine efficacy in these groups at highest risk for RSV-associated morbidity and mortality,” she argued. “[But] if vaccination is recommended for these groups, clinical trials will no longer be feasible for ethical reasons and we will have missed the opportunity to obtain the best level of evidence.”
Once a medical intervention is shown to be effective and is recommended for a population, it is no longer ethical to test it in a placebo-controlled trial.
There were also concerns about the fact that three people in the clinical trials done to test these vaccines developed Guillain-Barré syndrome after being vaccinated, a normally temporary condition in which people experience progressive paralysis.
Some vaccines are associated with a slightly elevated risk of GBS. Whether RSV vaccines are among them will not be clear until more people use them, but several members of the committee were clearly disconcerted by the possibility that there might be a link between these vaccines and GBS.
Committee members expressed worry about the fact that these vaccines will likely be given at the same time of the year as flu and Covid shots and it’s not yet clear if giving the vaccines at the same time undermines the immune responses they generate.
Studies of concomitant administration of Covid and RSV vaccines are still underway. A study that GSK conducted giving RSV vaccine at the same time as high-dose flu vaccine — a formulation recommended for older adults — showed the response generated against influenza as “non-inferior” to what was seen when flu vaccine was administered on its own, with the exception of the response to influenza A H3N2 viruses. Those viruses cause the worst flu illness in seniors and some members of the committee were concerned that giving these vaccines at the same time could hurt protection against influenza.
Given that both vaccines appear to offer protection over two RSV seasons, it remains to be seen how often older adults would need to be vaccinated against RSV. Likewise it is not clear whether people who are immunocompromised will be protected by these vaccines. Pfizer said it is currently conducting a study to see if one or two doses of vaccine would protect this population.
This story has been updated.