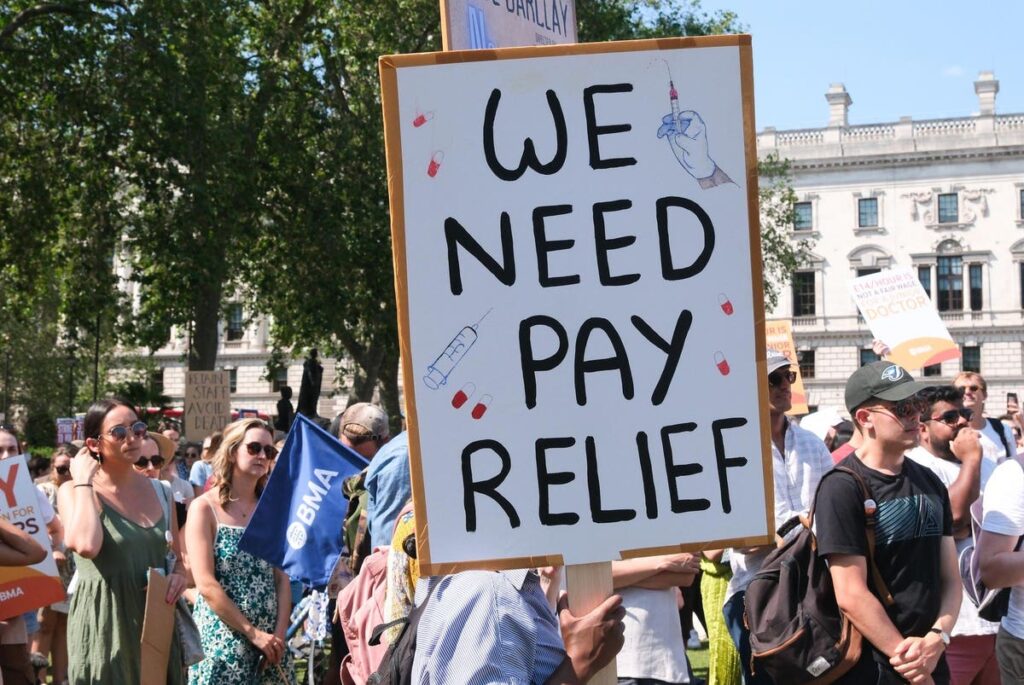
Junior doctors strike rally in Parliament Square, London, United Kingdom, June 16, 2023. (Photo … [+]
Junior doctors at England’s public health service are set to begin their longest strike yet, a week before their senior colleagues may stage their own walk-out.
Juniors will strike for five days from Thursday 13th to Tuesday 18th July unless they come to a pay agreement with government ministers. Senior doctors plan to walk out from July 20th to 22nd.
Leaders at the British Medical Association union argue doctors’ income has stalled for years as inflation has risen, leaving them with substantial real-terms pay cuts.
For hospitals, the strikes will mean cancelling swathes of routine appointments as senior doctors cover for their junior colleagues — and then walk out themselves.
Junior doctors are qualified physicians with up to 8 years’ hospital experience.
Their senior colleagues — known as “consultants” in the U.K. — are roughly equivalent to attending physicians in the U.S. They have never gone on strike before, and their specialist roles cannot be covered by other members of staff.
Junior doctors plan to strike in all hospital areas, including emergency and critical care, while seniors — known as consultants in the U.K., will offer a “Christmas Day”-level of service. They will still work in emergency care, but most routine procedures and appointments will have to be cancelled.
More than 600,000 appointments have already been cancelled over the last seven months of industrial action, which have seen staff including nurses, ambulance workers and physiotherapists walk out over pay concerns.
While other staff disputes have largely come to an end, doctors — who are paid according to a different framework — could continue striking for months if they do not come to an agreement with ministers.
Managers at some trusts fear they will struggle to run services safely during this latest period of industrial action.
The chief executive officer of a challenged West Midlands provider told their board this month that they were “extremely concerned about the impact on patients… as well as on the health and wellbeing of staff.”
As reported by the Health Service Journal, Worcestershire Acute Hospitals Trust CEO Matthew Hopkins wrote: “Junior doctors may only be recalled to work in the event of a mass casualty incident… Although other staff can cover for junior doctors they are becoming exhausted and increasingly reluctant to do so.
“We are therefore extremely concerned about our ability to maintain safe services.”
It isn’t just historically struggling trusts like Worcestershire Acute that are concerned aboutthe impact of ongoing strikes on care.
Dr Simon Steddon Chief Medical Officer at major London provider Guy’s and St Thomas’ Foundation Trust echoed similar concerns in a statement.
“The cumulative impact of this prolonged period of strike action by different professional bodies is now huge. To date, at our trust alone, we have already had to cancel or reschedule around 55,000 outpatient appointments and nearly 6,000 planned procedures,” he wrote.
As well as delaying care yet again for numerous patients, the walk-outs affect the wellbeing of hospital workers.
“Strikes also have a huge physical and emotional impact on our staff. The weeks before strikes are absorbed by reorganising services, negotiating staffing cover, making cancellations and rebooking patients,” Steddon added. “The response is exhausting. And the weeks after are spent catching up on pent-up demand, while trying to allow appropriate rest and recovery for staff.”
Both chief executives urged union leaders and ministers to end the ongoing dispute.
Why are doctors striking?
Union leaders say that junior doctor pay has fallen by 26% in real-terms since 2008/9 — although some organisations like the Institute for Fiscal Studies put that figure at between 11 to 16%. This disagreement comes from which measure of inflation is used.
In any case, union leaders say pay restoration is crucial not just to properly recognise today’s public sector doctors, but to ensure hospitals can recruit and retain staff moving forwards. The country’s public health workforce is already overstretched, and is likely to see increasing demand as the population ages.
Ministers argue that large pay increases are unaffordable and could themselves drive inflation.
But there is some hope for resolution from doctors north of the border.
Junior doctors in Scotland suspended planned industrial action this week when ministers offered a pay rise of 12.3%, as well as inflation-meeting increases for future years.