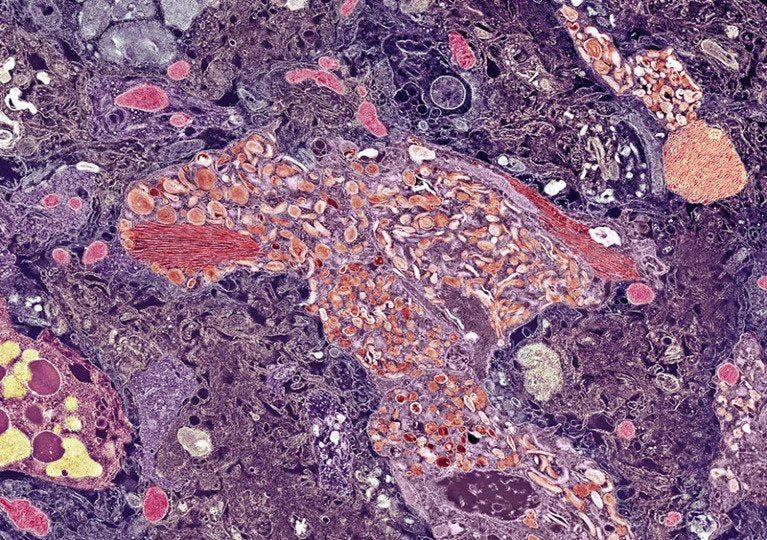
Electron-microscope image showing an amyloid plaque and tau fibres (dark pink lines) in the brain of … [+]
Neurologists have discovered a genetic mutation that may protect the brain from dementia.
Francisco Lopera, a researcher at the University of Antioquia in Colombia, has spent almost forty years studying a family of individuals with a rare form of early-onset Alzheimer’s disease that causes them to develop symptoms of dementia in their forties. The early form of Alzheimer’s disease is thought to be caused by the Paisa genetic mutation and is found in many of the 6,000 family members.
Now, Lopera has identified one family member who contains a second unique genetic mutation that has somehow protected him from dementia until the age of 67. Interestingly, despite his cognitive abilities, the patient carries the paisa mutation and displays other Alzheimer’s disease biomarkers like amyloid plaques.
This study not only challenges the theory that amyloid plaques are the primary cause of Alzheimer’s disease symptoms, but points to a potential avenue of treatment for Alzheimer’s disease. The question that remains is: what is this genetic mutation and how does it protect the brain from dementia?
This story begins with the paisa mutation. The paisa mutation is named after people from the Antioquia region of Colombia and is one of the most common genetic causes of early-onset Alzheimer’s disease. The mutation affects the PSEN1 gene which codes for a protein called presenilin 1. Presenilin 1 is part of a protein complex called gamma-secretase which is responsible for cutting other proteins into smaller pieces.
The gamma-secretase complex plays a crucial role in Alzheimer’s disease by cutting amyloid precursor protein. When the PSEN1 gene is mutated, the gamma-secretase complex has the tendency to cut amyloid precursor protein into slightly longer pieces. These longer chains of amyloid protein ultimately aggregate and form amyloid plaques in the brain.
It is believed that this mutation and its effects on amyloid plaque development is what causes many people in Antioquia, Colombia to develop early-onset Alzheimer’s disease. However, Lopera’s research now suggests that there may be more to the story of Alzheimer’s disease and dementia than just amyloid plaques.
Lopera and his research team approached their study by analyzing the genetic makeup of the 1,200 individuals within a Colombian family line that carried the paisa mutation. By studying the genetic makeup and profiles of the 1,200 individuals, they identified a subject who, unlike his family members, remained completely cognitively intact until the age of 67.
After imaging the man’s brain, researchers discovered that despite his cognitive abilities, he contained significantly higher levels of amyloid plaques. The researchers also examined another Alzheimer’s disease biomarker—tau tangles. Tau is another protein that has the tendency to aggregate in Alzheimer’s disease patients, leading to distinct tangles in the brain.
Interestingly, while the man exhibited higher levels of tau tangles across most of the brain, a particular region called the entorhinal cortex was left unscathed. The entorhinal cortex is believed to play an important role in learning and memory and is usually significantly damaged in those with severe Alzheimer’s disease.
This led to an important question: How was the man able to retain his cognitive abilities despite clear indicators of Alzheimer’s disease in his brain? Analysis of the man’s genetic makeup revealed that he contained a unique genetic mutation that affected his production of a protein called reelin.
In the adult brain, reelin is known to support the storage of long-term memories by protecting the formation of synapses—the connections between neurons. It also stimulates the growth and distribution of neurons. While studies have shown that genetic mutations which decrease reelin production can heighten the risk for schizophrenia and autism, very little is known about the protein’s role in neurodegenerative diseases like Alzheimer’s.
To examine the role of reelin and how the genetic mutation may affect cellular function in the brain, Lopera’s research team inserted the genetic mutation into mice. They found that the mutation increased the activity of reelin. In fact, the genetic mutation increased the number of neurons in the brains of male mice aged 6-12 months. This suggests that the reelin mutation may have a protective effect by promoting neuron growth and survival.
Lopera then assessed how the reelin mutation affected tau accumulation in the brain by inserting the reelin mutation into mice with the capability of developing phosphorylated tau. High levels of phosphorylated tau lead to an abundance of tau tangles. From this, they discovered that mice with the reelin mutation had a significant reduction of phosphorylated tau in not only the entorhinal cortex but the hippocampus—a broader region of the brain responsible for learning and memory. Beyond the hippocampus, the researchers found that tau phosphorylation was also reduced in the medulla oblongata which controls important processes like heartbeat, breathing, and blood pressure.
When researchers examined the molecular structure and interactions of the mutated reelin protein, they discovered something interesting. The mutated reelin protein actually binds to the same receptor as the APOE protein. The APOE gene is one of the few known genetic risk factors for Alzheimer’s disease. The fact that both the mutated reelin and APOE bind to the same receptors suggests that there may be some shared mechanisms between the two proteins. In other words, either a stronger protective reelin protein or a weaker APOE protein can provide protection against Alzheimer’s disease.
Lopera’s paper did not comment on the specific mutation in the reelin gene and how it may be altering reelin’s structure to increase the protein’s activity. However, Dr. Roberto Patarca, the Chief Medical Officer at ACCESS Health International, suggests that the mutation may impact three regions of the reelin gene that allow reelin protein to bind to the APOE protein. Mutations in these regions could make reelin more effective at binding to the APOE receptor, allowing the protein to have greater protective effects against APOE in Alzheimer’s disease.
This study is not the first to identify individuals that have severe amyloid plaques but do not experience symptoms of dementia. However, this paper is a significant stepping stone in locating a genetic mutation that may be responsible for protecting the brain from dementia in the presence of plaques. While more research must be done to determine exactly how and why the reelin protein seems to affect tau tangles in the hippocampus, this unique case may point to reelin as a useful target of Alzheimer’s disease treatments.