THE HEPATITIS C VIRUS
Hepatitis C is a serious blood borne disease that can cause severe liver damage and impacts over 2.5 million Americans. While the disease can be treated, treatment is not yet universally available and affordable to those who need it. With an estimated 66,700 new infections occurring in the United States each year, a hepatitis C vaccine would help to eliminate the disease from the United States and elsewhere. Current understanding of the natural history and greater variability of the hepatitis C virus means that the vaccine needs to be both broadly protective and long lasting. Is such a vaccine feasible? Here we outline the reasons for optimism despite the prevalence of hepatitis C variants which have confounded previous vaccine attempts.
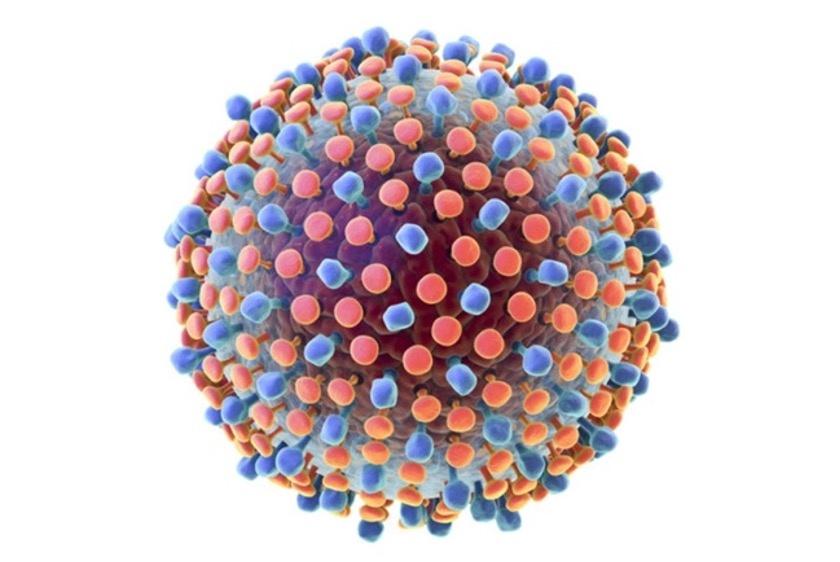
FIGURE 1. THE HEPATITIS C VIRUS HAS A HIGH DEGREE OF VARIABILITY. IT HAS SEVERAL GENOTYPES, EACH … [+]
Hepatitis C Variants: The Major Difficulty in Creating a Vaccine
The hepatitis C virus replicates rapidly and generates high variability resulting in multiple strains and subtypes. There are currently eight globally recognized hepatitis C genotypes with an estimated 30% variance of nucleotide divergence between them (Figure 1). Each genotype also carries multiple subtypes that can have up to 20% variance between them. For comparison, the hepatitis B virus, for which we do have a vaccine, has only an estimated 8% variance between genotypes. It is also important to note that the hepatitis C virus can cause superinfections. In these cases, an individual can be infected with multiple types or subtypes of the virus at the same time. Evidence suggests that infection with one strain does not protect against infections of another strain. The implication of this is that a vaccine would need to be broadly neutralizing against many different strains at the same time.
Reasons for Optimism
Despite the presenting challenges, there are reasons for optimism in creating a vaccine for hepatitis C. Around 30% of people who are infected with the hepatitis C virus do mount an effective immune response that protects them from disease and clears the infection on its own. The study of these people reveals two major factors about their immune responses: they produce broadly neutralizing antibodies, and they make robust and sustained T-cell responses (Figure 2). The knowledge of how these people can control and clear the infection offers valuable insight for creating a successful vaccine.
FIGURE 2. ALTHOUGH ABOUT A THIRD OF THOSE WITH HEPATITIS C CAN CLEAR THE INFECTION ON THEIR OWN BY … [+]
Considerations for a Broadly Neutralizing Vaccine
An effective hepatitis C vaccine must first generate broadly neutralizing antibodies and second, elicit long term memory T-cells. In the antibody immune response, B-cells can induce the production of broadly neutralizing antibodies. These specialized antibodies are useful because they can recognize and block viral entry across multiple strains of hepatitis C. In addition to those antibodies, it is also important that the vaccine initiate robust T-cell immune responses. When an adaptive cell-mediated response starts taking effect, the immune system releases two types of T-cells: helper CD4+ cells, which prompt B-cells to make antibodies, and cytotoxic CD8+ cells which kill cells already infected with the hepatitis C virus. Sustained memory T-cells are an important part of clearing current hepatitis C infections and preventing reinfections. Fortunately, we can take lessons from earlier vaccines like the ones we have for the respiratory syncytial virus and the Ebola virus that show that if you understand pre-fusion complexes and conserved epitopes, you can make broadly neutralizing antibodies and strong T-cell responses.
Conserved T-Cell Epitopes
One method that vaccines, like the Ebola vaccine, use to induce production of T-cells is by targeting conserved epitopes. An epitope is a specific part on the surface of a virus that T-cells can bind to and signal B-cells to produce hepatitis C antigen specific antibodies. Conserved epitopes are T-cell targets that appear across multiple strains of hepatitis C which would allow the vaccine to work against a breadth of antigen variants (Figure 3). Studying the antigens of individuals who have spontaneously cleared the hepatitis C virus can offer hints as to which conserved epitopes might be the most useful in inducing the best T-cell responses. This method was also integral to developing a pan-genotypic COVID-19 vaccine.
FIGURE 3. FINDING THE CONSERVED EPITOPES OF THE HEPATITIS C VIRUS WILL HELP DEVELOP A BROADLY … [+]
Pre-Fusion Complexes
The success of the respiratory syncytial virus vaccine offers insight into pre-fusion complexes and how they generate broadly neutralizing antibodies. To fuse with and infect liver cells, the surface proteins of the hepatitis C virus must undergo a conformational change. Broadly neutralizing antibodies prevent viral infection by binding to epitopes on virus’ surface proteins and blocking the conformational shift from occurring. Locking the virus in its pre-fusion state can then prompt the production of more broadly neutralizing antibodies (Figure 4). A vaccine that contains these pre-fusion antigens would produce large amounts of broadly neutralizing antibodies that not only recognize conserved epitopes, but also bind across multiple targets on the virus’ surface proteins. Current research focuses on the AR4 epitope and how it may lock the E1-E2 hepatitis C protein in its pre-fusion form to block the ability to fuse with liver cells (Link).
FIGURE 4. AS WE’VE LEARNED FROM THE DEVELOPMENT OF THE RESPIRATORY SYNCYTIAL VIRUS VACCINE, BROADLY … [+]
What Methods of Vaccine Delivery Are Being Considered?
The final consideration for creating a successful hepatitis C vaccine is the design of the vector. There are several methods currently being explored, some of which are more suited for antibody immunity while others are better suited for triggering a cell mediated immune response. One option for delivery is using mRNA as a vector. These types of vaccines use a lipid coating or inactive virus shell to transfer viral RNA into cells to teach them how to make effective antibodies. Another approach relies on subunit vaccines, purified proteins or peptides combined with potent adjuvants. Still others depend on viral vectors such as the family of adeno-associated viruses to deliver the antigens.
While we don’t know if these methods will be successful, the current efforts underway are promising. In the meantime, we must rely on the implementation of programs like the 100 Million Healthy Lives initiative in Egypt and the expansion of efforts to lower the costs of hepatitis C drugs.