When seriously depressed patients don’t respond to antidepressants, the alternatives are limited. Now a new study has found that ketamine performs at least as well as the current gold standard for such patients, electroconvulsive therapy (ECT), suggesting it deserves consideration as a frontline response for people with treatment-resistant depression.
But while the potential benefits are comparable and ketamine is easier to administer than ECT, the addiction risks of long-term ketamine treatments aren’t well established, leading some physicians to urge caution. “It’s a question of risk assessment for each individual patient,” said Boris Heifets, who studies ketamine at Stanford University and was not involved in the new research. “Neither of these things is risk-free, neither is transformative.”
The findings, presented Wednesday at the American Psychiatric Association meeting and published in the New England Journal of Medicine, found intravenous ketamine was “not inferior” to ECT. Patients randomly assigned to take ketamine twice a week for three weeks actually had slightly better results, with 55.4% responding to treatment. That compared to a 41.2% response rate for those who had ECT three times per week over the same period.
The study, with 403 participants, was significantly larger than previous ketamine comparison studies; a meta-analysis of these smaller studies, published last year and focused on major depression rather than treatment-resistant depression, found ECT had better results. But the new paper is both better-powered and arguably focused on sicker patients, only enrolling those with major depression without psychosis who didn’t respond to SSRIs, providing strong evidence of ketamine’s equivalence to ECT. A long-time anesthetic, ketamine has gained popularity in recent years as a treatment for depression.
The implications of the findings are “huge,” said Patrick Oliver, medical director at MindPeace ketamine clinics who has researched the drug as treatment for depression but was not involved in the study. Though it was structured to show “non-inferiority,” he said the data suggest ketamine worked better than ECT.
“I would say hands down that this should change the practice of interventional psychiatry,” said Oliver, bringing ketamine from last to first choice for patients who don’t respond to SSRIs. That said, he added, neither results are great. “We’re at a C-minus.”
Others, though, were more reserved about ketamine’s future use, pointing to its addictive potential. ECT, which is performed while the patient is under general anesthesia, is hardly risk-free, having been shown to cause cognitive impairment including long-term memory loss. Ketamine, by contrast, is known to be addictive though the exact risks are not well-researched. Without regulation or more data, some worry that widespread ketamine use could lead to another addiction epidemic like the opioid crisis.
“The follow-up period of the current trial was not long, nor did it assess future drug-seeking behavior among those who did or did not have a response to ketamine,” Robert Freedman, psychiatry professor at the University of Colorado Denver School of Medicine, wrote in a NEJM editorial published alongside the study. “We need to remember that only a minority of physicians were responsible for the oxycodone epidemic.”
Amit Anand, lead author of the study and a psychiatrist at Brigham and Women’s Hospital in Boston, said there was minimal evidence of addictive potential, especially at the trial’s subanesthetic dose of 0.5 milligrams per kilogram of body weight. “I don’t think there’s any firm data people are abusing it,” he said. “But we have to keep it in mind.”
In the study, though, 41% of participants assigned to take ketamine continued to do so during a six-month follow-up period. “That to me is a warning,” said Heifets, adding it’s not a short-term “we fix you and you’re done” treatment. ”This is a subscription model.”
Both ketamine and ECT are fast-acting for patients in acute distress, which is extremely valuable for an emergency setting. But Anand agreed that the longer-term use of ketamine hasn’t been well-studied. “The challenges with ECT and ketamine are, you can get an acute response, but how do you actually maintain it?”
Ketamine, which in higher doses is popular as the “Special K” party drug, can also cause bladder damage in some patients.
Freedman called for detailed informed consent, while Heifets said there should be regulation on how the medication is dispensed, and careful monitoring of those who take ketamine long term. Both warned of lessons that should be learned from the opioid crisis. “Why do we think ketamine’s going to be different? If you ignore risks and expand access as aggressively as you can, we’re going to be in the same place in 10 years,” said Heifets. “Ketamine is not oxycodone. But it does have an abuse liability. Even if it’s relatively modest, if you give it to enough people, the math is upsetting.”
That said, these concerns need to be balanced against ECT’s potential for memory loss. ECT is linked with long-term cognitive problems, including permanent memory loss, for some patients. Patients in the study temporarily had worse memory recall following ECT treatment, but improved during the six-month follow up. They also were more likely to have musculoskeletal adverse events, whereas dissociation was reported as a side effect for patients receiving ketamine.
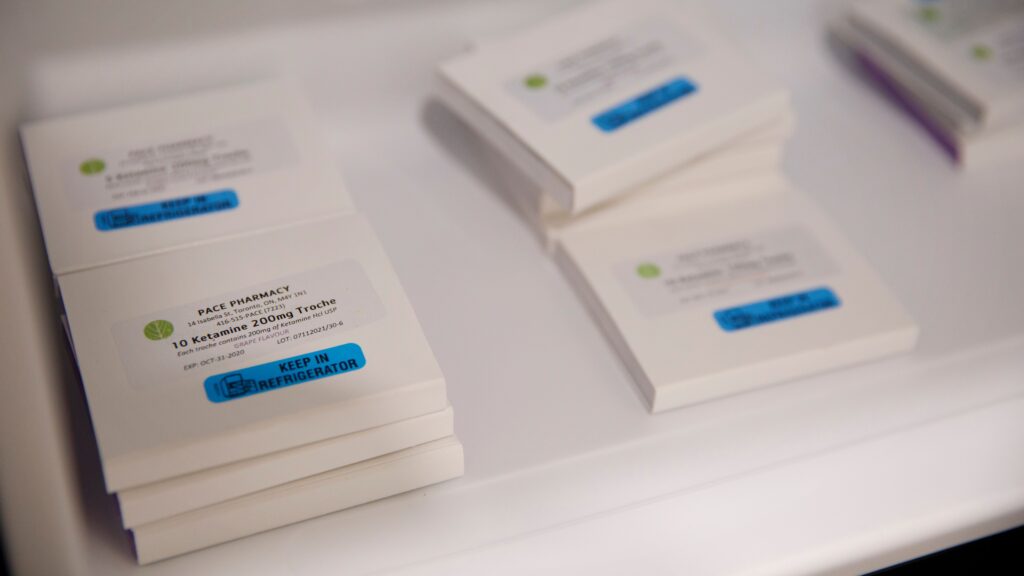
Ketamine is not approved as a depression treatment, despite evidence around its efficacy; the drug is generic, meaning there’s no financial incentive for a drugmaker to take on the costs of submitting ketamine to the Food and Drug Administration for approval. Instead, esketamine, a modified version of ketamine patented by Janssen Pharmaceuticals, a subsidiary of Johnson & Johnson, has been approved as depression treatment. This drug costs more but, unlike ketamine, can be covered by insurance.
The study’s author, Anand, agreed with Oliver’s view that ketamine could be tried ahead of ECT. “There’s an equal chance you’ll get better with ketamine,” he said. The results are strong enough, he said, to prompt insurers to consider covering ketamine despite the lack of FDA approval.
That would give patients and physicians more options. “It becomes a matter of which side effects are you more comfortable with,” said Heifets. “Neither of these treatments is perfect.”