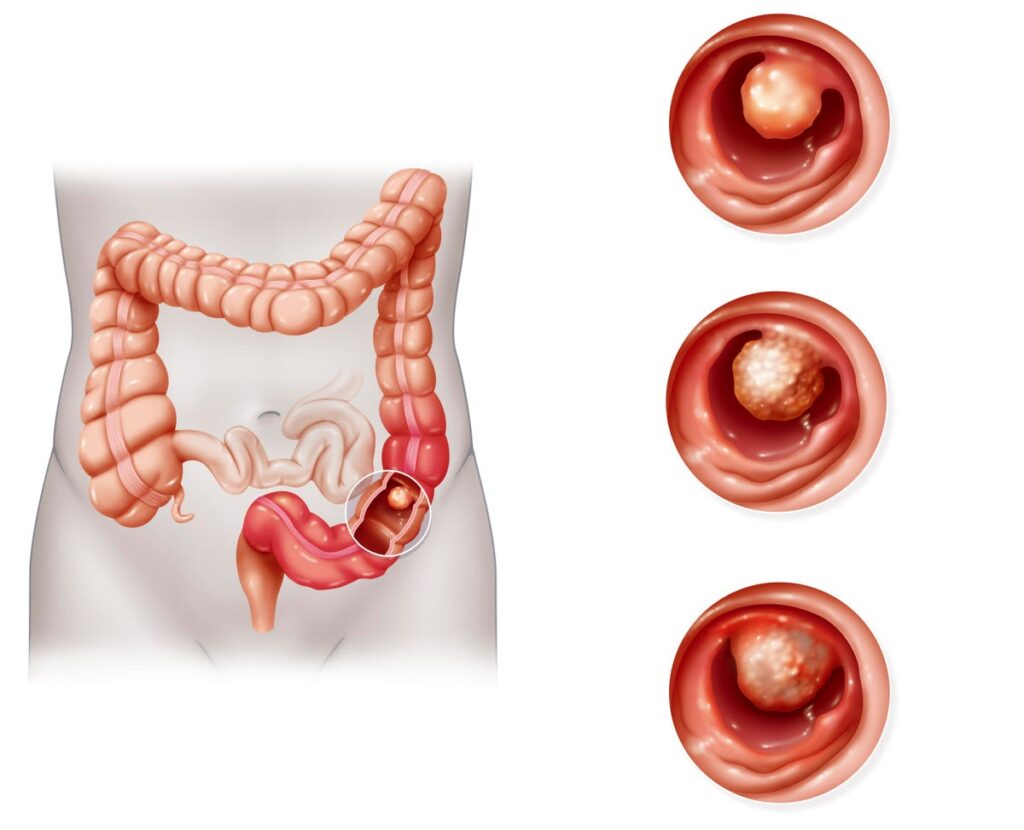
Illustration of colon cancer. The cancer develops on the colon’s mucus membrane. In 70% of cases, … [+]
“I never would have found it early if I hadn’t been screened”.
These are the words of Robert, a colorectal cancer survivor whose story is highlighted on the CDC website. Because his father was diagnosed with colon cancer at the age of 45, he urged his doctors to investigate whether this was a possibility for him. Aside from occasionally feeling tired, Robert had no symptoms of colon cancer. Screening tests subsequently showed a positive diagnosis of colon cancer for Robert at the age of 51. He then underwent surgery to remove the cancer that then saved his life.
March is colorectal cancer awareness month so it should behoove us to learn more about it. Robert is one of many Americans that have been diagnosed with colorectal cancer, a cancer that involves the digestive tract, specifically the colon and rectum. In fact, in 2023 alone, there have already been 106,970 new cases of colon cancer diagnosed in America, and 46,050 new cases of rectal cancer, according to the American College of Surgeons. Colorectal cancer is the second leading cause of cancer death in America only behind lung cancer. In 2022, 52,580 Americans died of colorectal cancer, according to the American Association for Cancer Research.
As Robert’s case illustrates, screening for cancer is pivotal for survival, since symptoms for cancer are not always present. According to the US Preventive Services Task Force, most adults should be screened for colorectal cancer beginning at age 45. There are many different available options to screen for colorectal cancer, but the gold standard is colonoscopy, which should be performed every 10 years for those that do not have an increased risk of colorectal cancer. In this test, your doctor will insert a thin, flexible lighted tube into your rectum to check for polyps and/or cancer in your colon and rectum. The advantage of this test is that your doctor can remove some polyps and even cancers in real-time during the exam. Alternatives to a colonoscopy include a virtual colonoscopy which uses x-rays and computer technology to create images of your colon and rectum, that then get reviewed by a radiologist physician to detect any possible polyps or cancer. There are also stool tests that can be performed annually in the comfort of your home such as the fecal occult blood test and the fecal immunochemical test. If a virtual colonoscopy or stool test is positive, a colonoscopy is usually still needed to complete the screening process.
Importantly, there are racial disparities that exist with respect to mortality and screening of colorectal cancer. For example, according to Kaiser Family Foundation, Black patients have the highest rate of new colorectal cancer diagnosis of all racial groups, followed by White patients and Hispanic patients. In addition, despite improvements in screening access that have occurred from national policies like the Affordable Care Act, racial disparities for colorectal cancer screening still persist. For example, according to a study in Clinical Gastroenterology and Hepatology, between 2008 and 2016, screening rates for colorectal cancer have been highest amongst White Americans and lowest for Hispanic Americans. By the end of the study period, screening rates for Hispanic Americans were 17% lower than White Americans, while screening rates for Black Americans were 4% lower than White Americans.
Given the racial disparities that exist with respect to mortality and screening for colorectal cancer, we must improve this gap to allow all American citizens to benefit from screening processes. Screening remains the number one method of detecting cancer early and saving lives, as colorectal cancer has a 90% survival rate when detected early. Bolstering education of screening through media outlets can go a long way in increasing the awareness that is necessary to bring Americans to their doctors to get screened. At-home screening stool tests should also be made widely available, particularly to Black Americans and Hispanic Americans that have had less than optimal screening rates for this deadly cancer.
As Robert states, “People tell me that they are scared to get screened, but I think it’s scarier if you have a tumor that the doctor can’t remove”. Getting screened for colorectal cancer could literally be the difference between life and death, as it was for Robert.