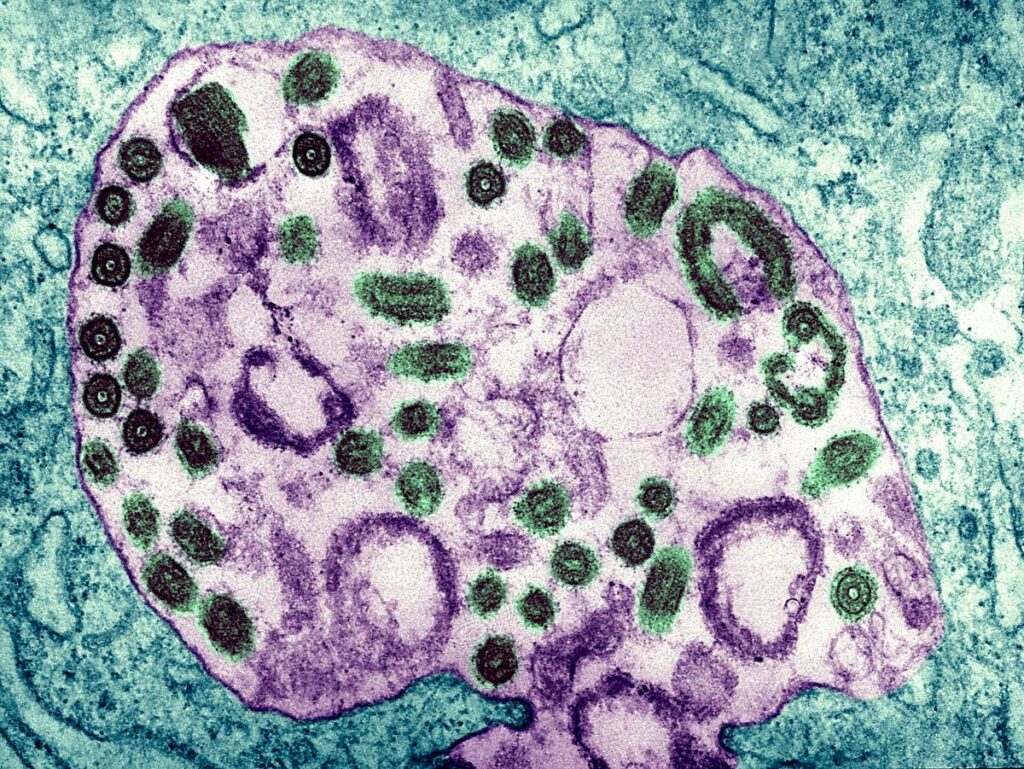
Electron Micrograph Of The Marburg Virus. Marburg Virus, First Recognized In 1967, Causes A Sever … [+]
Equatorial Guinea has just confirmed its first outbreak of Marburg virus, one of the families of hemorrhagic fevers related to Ebola. As with last year’s outbreak in Ghana, patient specimens had to be sent to the Institut Pasteur in Senegal for confirmation, as it requires specialized testing. One of eight samples has been confirmed thus far. There have been 16 suspected cases and 9 deaths so far.
Symptoms of Marburg are nonspecific and include (the often abrupt onset of) fever, headache, nausea, vomiting and diarrhea, so it might be confused with many other infections. When there is blood in the emesis or stool, the diagnosis of a hemorrhagic fever becomes much clearer. The incubation period is from 2-21 days.
Like Ebola, Marburg can be quite deadly, with an 88% fatality rate. Unlike Ebola, we have no vaccines to protect people yet, or other specific treatments. Monoclonal antibodies have been used to successfully treat some people ill with Ebola, with a moderate reduction in death, from 49.4% to 35.1% for Ebanga (Ansuvimab-zykl) treatment. The vaccine for Ebola offered a 97.5% protection rate in the 2018-20 outbreak in the Democratic Republic of Congo, which was due to the Ebola Zaire strain.
The most recent outbreak of Ebola in Africa occurred in Uganda in September 2022. It was due to a different strain, Ebola Sudan, for which we have no vaccines or specific treatment.
For Marburg, Ebola Sudan, and other hemorrhagic fevers, treatment is supportive by providing fluids and electrolytes to avoid shock.
The primary focus now will be controlling the spread of the infection, which occurs through these infected secretions or contaminated surfaces, and by quarantine. Patients who are symptomatic need to be carefully isolated. The WHO and local officials will provide education on infection control and supplies of gowns and gloves (PPE). Contact with bodies is common in many cultures and has previously been a source of transmission.
Marburg has now been seen in Ghana, Angola, Uganda, the Democratic Republic of the Congo, Kenya, and South Africa. The first outbreak was seen in 1967 in Germany and Serbia. It came from the importation of green monkeys from Angola. A quarter of the 31 people infected died. Subsequently, there were larger outbreaks in the DRC in 1998-2000, with 152 people and 83% mortality. The largest outbreak was in 2005 in Angola. There were 252 cases and a 90% death rate. This was thought to be caused by reusing contaminated transfusion equipment between patients.
Egyptian Rousette bats, which live in caves and mines, are reservoirs for the Marburg virus. There have been infections among Uganda miners in 2007 from the Python Cave in Uganda. Subsequently, two tourists became infected from the same site, where they had gone caving. Bat guano or infected aerosols were the likely sources of transmission.
One of the problems with Marburg, as with other animal-related infections (zoonosis), is that there is limited surveillance and diagnostic tests; until there is an outbreak, early cases are likely to be missed.
Many of these events—called spillover events—occur because we encroach on wildlife. As we do this more—be it in mining, deforestation for cattle, or other disruptions of the environment, we can expect to see more such outbreaks.