Of the 103 million confirmed cases of Covid-19 in the U.S., an estimated one-third have led to long Covid — a condition that ranges in severity, but can be debilitating. A new study suggests that even more people may be suffering from the post-viral syndrome without having ever received an official diagnosis of Covid-19.
The study, published Wednesday in Neurology, Neuroimmunology & Neuroinflammation, was small, examining only 29 patients. But it offers unique insights into how many cases of long Covid may go unidentified because the patient’s Covid-19 infection wasn’t detected.
“We estimated that there were approximately 10 million people in the first year of the pandemic in the U.S. who are in this predicament: who got Covid, got long Covid, but tested negative for Covid,” said Igor Koralnik, who led the study and is the chief of the division of neuroinfectious diseases and global neurology at Northwestern Medicine.
The findings of the study suggest that a positive diagnosis for Covid-19 should not be a requirement for treating people whose symptoms are in line with long Covid, said Ziyad Al-Aly, a clinical epidemiologist at Washington University in St. Louis, who was not involved with the study.
“Restricting access to care [for] long Covid to people who had established disease will disenfranchise and really marginalize people who are actually likely the most vulnerable among us,” said Al-Aly, noting that people with fewer resources or who live in areas where testing is not easily available may have a harder time getting a diagnosis.
Koralnik, who oversees Northwestern’s Neuro Covid-19 Clinic, also noted that “negative long-haulers” should be included in long Covid trials and studies, from which they are currently excluded.
Roughly two-thirds of Covid-19 clinics in the country do not accept long Covid patients without a known diagnosis of the virus — but Koralnik’s does. This gave him the opportunity to do further testing on 29 of the patients treated there who hadn’t tested positive for Covid but had long Covid symptoms. He found that 41% of patients who reported symptoms but hadn’t tested positive at the time of the infection had T cell responses or antibody responses to Covid-19, meaning they had been exposed to the virus.
Patients who had long Covid without an official diagnosis faced treatment delays, receiving clinical evaluation at Koralnik’s clinic at an average of 10.7 months after the onset of symptoms, compared to evaluations at an average of 5.4 months after onset of symptoms for people who had tested positive for Covid-19.
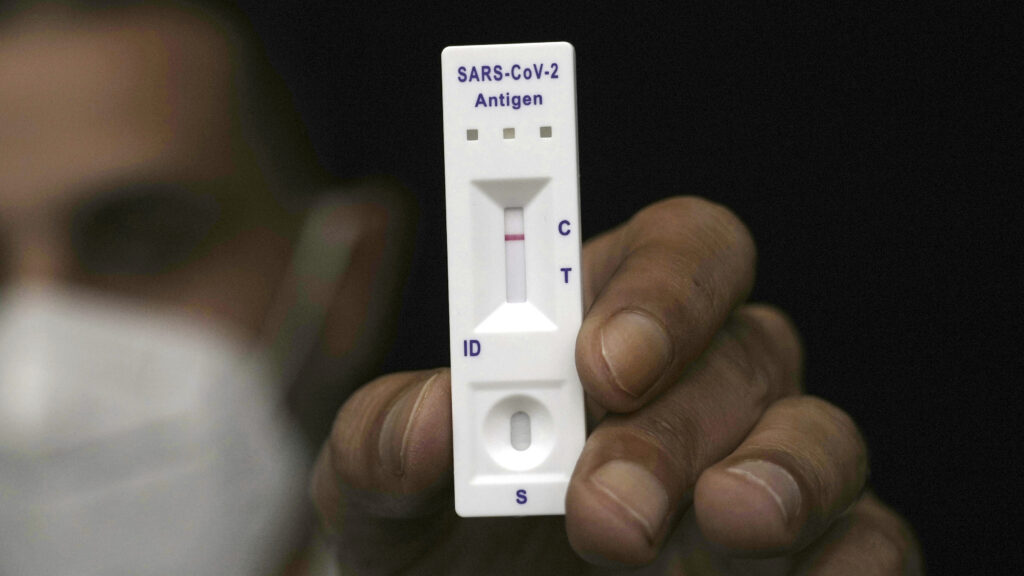
Many of the missed cases can be attributed to the fact that Covid testing was limited at the beginning of the pandemic. At-home nasal swab kits weren’t yet available, said Koralnik, and because blood tests were calibrated to the levels of antibodies in people hospitalized with severe pneumonia related to Covid, they missed milder infections.
All this meant that many people who had mild or asymptomatic infections at home never received an official diagnosis, nor did people who were tested in the hospital weeks after they had first developed symptoms. Yet some of these people went on to develop post-viral syndrome symptoms that were consistent with those of Covid-19 long haulers, said Koralnik.
“They have the same presentation, the same type of symptoms. They are almost indistinguishable,” he said.
Many of these patients have a hard time even getting their symptoms acknowledged. “They felt sometimes very disenfranchised or gaslighted even, because people told them, it’s all in your head, it’s stress, anxiety, it’s going to get better, you can do yoga and relaxation,” said Koralnik. “But in fact we can show that at least 40% of this small sample were really exposed to the virus. So it would be vindicating for those people to know that one.”
“It’s really refreshing and wonderful to actually see data showing this,” said Al-Aly. “It really supports our thinking that there are people in the community who are suffering from post-acute sequelae of SARS-CoV-2 who don’t have a formal diagnosis of Covid-19 and it doesn’t make the disease any less real.”
The study also highlights the pervasiveness of long Covid at a time when there’s increasingly less public focus on the disease.
“We have a crisis on our hands. But unfortunately, in a lot of ways it’s really invisible to the average person on the street, because a lot of these long Covid patients who are actually severely impacted are in bed or at home,” said Al-Aly. “[They are] the missing millions among us who are missing in the workforce, missing from parties, missing from birthdays.”
“Long Covid is really a pandemic within the pandemic,” said Koralnik.