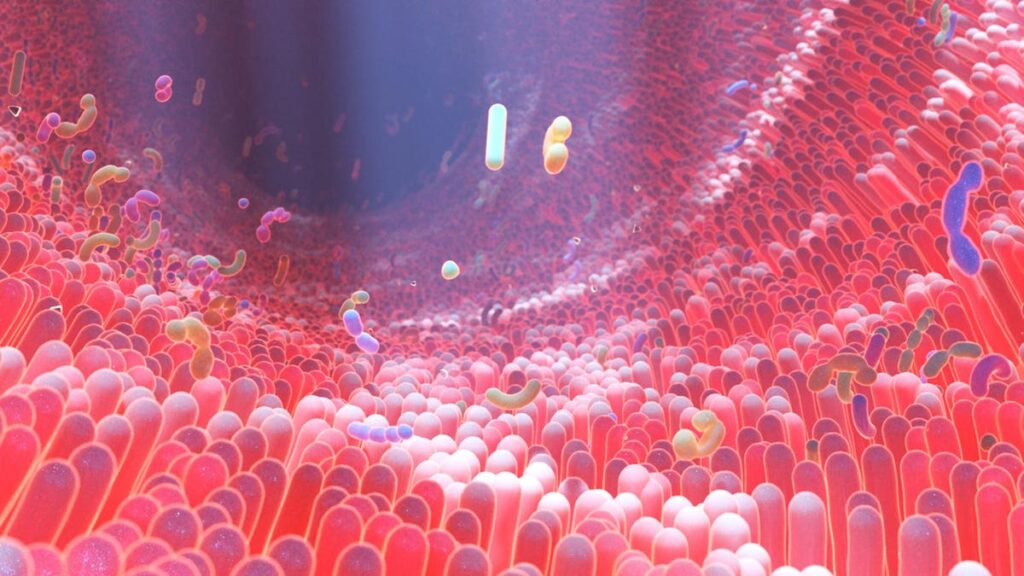
3D rendering of human intestine villi and microbiome
Ten years ago, the researcher Phil Strandwitz was giving a talk at Harvard University regarding a new paper discussing a potential link between the gut microbiome and the developing brain. In particular, he wanted to highlight how a small group of scientists were examining whether the gut may play a role in autism spectrum disorder.
“There was somebody in the front row who just slammed their book shut and said, ‘This is impossible, microbes can’t influence the brain,” remembers Strandwitz, now CEO of Cambridge, Massachusetts-based biotech Holobiome. “Now, if you go to any neuroscience conference there are almost always microbiologists there.”
While the connection between the gut and the central nervous system was once considered speculative, prestigious journals like Science are now publishing papers on how gut microbes can influence the brain and behavior.
In 2019, academics at the Weizmann Institute of Science in Israel published a landmark study in Nature where they showed that the gut microbiome may affect the course of the incurable neurodegenerative disease amyotrophic lateral sclerosis (ALS). Disease progression in mice, whose genomes had been altered to create an ALS-like illness, slowed after they received either certain strains of gut microbes or metabolites known to be secreted by those microbes. Further studies have followed, linking the microbiome to other neurological diseases and disorders.
“There’s a really good chance that the connectivity between our microbes and us could explain, at least in some cases, depression, symptoms of Parkinson’s, recovery from stroke, pain and even risk of dementia, a wide range of different things that are classically considered neurological in origin,” says Strandwitz.
Understanding The Gut/Brain Axis
At the simplest level, we now know that microbes in the intestines can communicate directly with the CNS through the vagus nerve, which senses activity throughout the gastrointestinal (GI) tract and runs from the gut to the brain. Through this connection they may be capable of modulating neuroinflammation as well as the levels of neuroactive molecules such as neurotransmitters and neuropeptides which drive complex behaviors relating to emotions and anxiety.
In addition, Strandwitz says that microbes continuously produce proteins and other molecules which are absorbed into the bloodstream, where they can influence the localized immune system and the peripheral nervous system. According to John Cryan, a professor and microbiome researcher at University College Cork, some of these microbial metabolites may also play a role in regulating the blood-brain barrier, the thin layer of cells that separates the brain from the periphery. A more permeable blood-brain barrier would allow toxins and other infections to reach the brain, potentially contributing to some neurodegenerative disorders.
“Right now, there’s a lot of interest in how the microbiome could shape the integrity of the blood-brain barrier, which could have implications for many disorders from Alzheimer’s to epilepsy,” says Cryan. “For epilepsy, anything that changes the balance between inhibition and excitation could be playing a role, which is why the microbiome could be involved.”
The most successful non-pharmacological treatment for epilepsy has long been the ketogenic diet and in recent years research has begun to suggest that the diet’s renowned anti-seizure effects are in fact mediated by the microbiome.
Now San Diego-based biotech Bloom Science, which has received an investment from my team at Leaps, has developed a new oral therapeutic that aims to replicate the antiepileptic effects of the ketogenic diet in children with Dravet syndrome, a rare form of epilepsy. The therapeutic contains two gut microbes which have been found in both cell-based assays and animal studies to reduce neuronal hyperexcitability, which increases risk of seizures, and increase the levels of a neurotransmitter called gamma aminobutyric acid (GABA) in the hippocampus. Low levels of GABA are also linked to seizures.
Through boosting GABA and modulating other key bioenergetic pathways, the hope is that this intervention can significantly reduce seizure frequency and duration, and perhaps even eliminate seizures. Last month, Bloom announced positive results from a Phase 1 safety trial in healthy adult volunteers which showed that it was well tolerated with no serious adverse events. The company has since received Rare Pediatric Disease Designation for this oral therapeutic from the FDA for Dravet syndrome and intends to progress to a Phase 2 clinical trial next year.
Bloom is also investigating whether this same oral therapeutic can offer clinical benefits for patients with ALS through addressing the underlying oxidative stress that is a critical factor in the progression of the disease. Preclinical studies using mouse models of ALS have shown that this therapeutic can attenuate motor neuron loss as well as increase lifespan and motor coordination in these mice. The company intends to conduct a Phase 2 clinical trial in ALS patients next year. Future plans also include developing microbiome-based therapies to address anxiety and depression.
Alleviating Symptoms of Autism Spectrum Disorder
One of the first microbiome-targeting drugs that may become clinically available for a neurological condition could be a therapy aimed at treating ASD-associated irritability, which can include aggression, severe tantrums, or the need for isolation.
Autistic children have long been known to have differences in their gut microbiota and as a result are more susceptible to GI issues compared with their neurotypical peers. According to Stew Campbell, CEO of Woburn, Massachusetts-based Axial Therapeutics, irritability in children with ASD represents a considerable unmet need and is thought to be exacerbated by these underlying differences in the gut.
Last year, a team of researchers led by Axial Therapeutics’ scientific founder, professor Sarkis Mazmanian at California Institute of Technology, demonstrated in mice how bacteria-derived metabolites in the gut can reach the brain via the bloodstream and alter communication networks associated with anxious behavior.
The company has developed an experimental product they describe as a tasteless and odorless powder formulation that can be mixed with soft food and taken orally. It is designed to bind to these metabolites in the gut before they can get into circulation. Right now, the product is in a Phase 2b study conducted across multiple centers in the United States, Australia and New Zealand, with data anticipated to be reported in the first quarter of 2024.
The Size Challenge
Yet there are still considerable challenges. According to Nik Sharma, CEO of London-based biotech BioCorteX, one of the major ones when it comes to potentially using the gut microbiome to alter the path of neurological disorders, is its sheer size.
“The numbers [of microbes] are astronomical,” says Sharma. “It’s probably not going to be one individual species of bacteria which is driving any of these diseases, it’s probably going to be a consequence of the interactions between millions of microbes.”
BioCorteX are now looking to apply mathematical modelling to better understand how a particular therapeutic might impact the entire ecosystem of microbial species within the gut, with the aim of yielding insights that could improve the design of future drugs.
“We don’t just look at the bacteria, but also viruses and fungi in the gut, and they all interact to some extent,” says Sharma. “This is important to model because for example you could try to medicate with a bacteria, but that bacteria isn’t going to do very well if surrounding phages – viruses which attack a particular species of bacteria – act to keep it in check.”
As the science advances, I am optimistic that targeting the microbiome will provide a novel way of tackling some of the most devastating neurodegenerative conditions.
Sharma is particularly passionate about trying to make an impact in the field of ALS. “That’s my specialist clinical area and it’s a terrible disease,” he says. “We know that the gut microbiome is intimately connected with the microglia, brain cells which are detrimental later on in the process of these neurodegenerative diseases. There’s a lot of hurdles to overcome before we can do this, but I think that connection between the microbiome and those microglia will be an attractive target to go after.”
Thank you to David Cox for additional research and reporting on this article. I’m the head of Leaps by Bayer, the impact investment arm of Bayer AG. We invest in teams pursuing fundamental breakthroughs in life science, targeting ten huge challenges or “leaps” facing humanity, including to protect brain and mind.