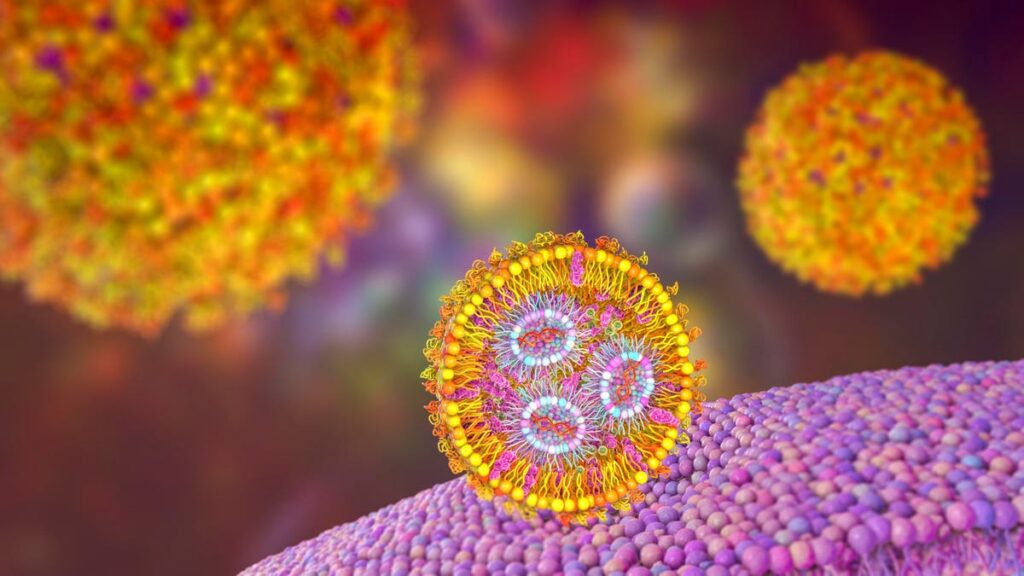
Lipid nanoparticle mRNA vaccine. A type of vaccine used against Covid-19 and influenza. 3D … [+]
This story is part of a series on the current progression in Regenerative Medicine. This piece discusses advances in stem cell gene therapy.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
mRNA technology is ushering waves in stem cell gene therapy. A preclinical study published in Science showcases three exciting findings demonstrating how mRNA-based innovations could make treating and curing genetic blood diseases simpler and safer than the current treatment standard. As part of a three-part series, this installment will explore how mRNA could replace toxic chemotherapy and radiation procedures. Future installments will describe how the researchers corrected problematic gene mutations at their source and genetically altered blood stem cells in vivo with the same platform.
The Current Treatment Standard
Genetic blood disorders encompass many diseases that impact the blood, including sickle cell anemia and thalassemia. Such conditions arise when the genes responsible for producing essential proteins in blood cells mutate or become abnormal. These protein abnormalities affect blood cell development and are typically hereditary—meaning they are passed down from parent to child through genetic inheritance.
One way to correct the irregular blood cell production is to address the source: hematopoietic stem cells. All blood cells in the body, functioning or otherwise, develop from these immature blood stem cells (Figure 1). Replacing the aberrant, disease-causing stem cells with healthy ones allows the body to repopulate with healthy blood cells. This procedure is known as hematopoietic stem cell transplantation or bone marrow transplant.
Figure 1: All blood cells originate and develop from hematopoietic stem cells. Hematopoeitic stem … [+]
Risks of Stem Cell Transplantation
Stem cell transplantation can treat and cure, but the process incurs certain risks. For example, high-dose chemotherapy or radiation may be used to suppress the patient’s immune system, leaving space for the transplanted cells to engraft and establish themselves. These conditioning methods are toxic to healthy cells, increasing the risk of long-term complications such as organ damage or failure. Damage often targets the lungs, liver and reproductive organs. Researchers hope to develop a new ablation method that significantly reduces this associated toxicity.
mRNA: a Less Toxic Alternative
Researchers at the University of Pennsylvania turned to mRNA technology as a potentially less toxic solution to deplete stem cells. mRNA-based innovations offer a favorable safety profile, precise targeting and a general flexibility that could benefit a variety of treatments—be it vaccines, CAR T therapy or blood stem cell transplantation, as shown through this study.
Attuned for Ablation
In basic terms, mRNA technology is a delivery system for genetic information (Figure 2). Lipid nanoparticles encapsulate and transport the desired mRNA to a specific cellular destination. Upon arrival, the target cell will engulf the nanoparticle; the nanoparticle will degrade and release the mRNA cargo; and the target cell will produce proteins based on the released genetic instructions.
Several key changes were needed to adapt the platform for blood stem cell ablation. mRNA technology relies on antibodies to direct to the vehicle to the right cell target. The study authors determined that antibodies against surface protein CD117 worked better than anti-CD47 antibodies at targeting hematopoietic stem cells. Anti-CD117 antibodies were then attached to the lipid nanoparticles via SATA-maleimide chemistry. The process alters the nanoparticles to have maleimide groups and the antibodies with sulfhydryl groups. The two groups act as a molecular hook and loop, easily connecting together to form a strong link.
Next, the nanoparticles were designed to carry synthetic mRNA that promotes controlled cell death in stem cells; the encoded gene is called PUMA, short for p53 up-regulated modulator of apoptosis. If the delivery is successful, the mRNA should initiate a self-destruction pathway in the cells, thus culling functional stem cell numbers in the bone marrow.
Figure 2: mRNA technology relies on antibody-decorated lipid nanoparticles to deliver the desired … [+]
Mouse Model Results
Researchers tested their CD117-targeted, mRNA-carrying lipid nanoparticles in cell culture and mice models. The series of experiments illustrate this platform’s potential to safely target and deplete hematopeitic stem cells.
The team treated one set of bone marrow cells with CD117-targeting PUMA lipid nanoparticles and left another set untreated. These cells were injected at equal or increasing ratios into mice with a reduced number of bone marrow cells. Within two weeks, the mice that received high nanoparticle ratios die from transplanation from bone marrow failure—a positive sign for stem cell depletion. In contrast, the mice injected with higher proportions of untreated bone marrow cells live up to the four month endpoint. They do not undergo thorough ablation and maintain higher blood cell counts.
This result was echoed with in vivo testing. Blood stem cell numbers reduce significantly six days after mice receive a small dose of the PUMA-carrying lipid nanoparticles.
Could the nanoparticles be used to prep mice for stem cell transplantation? To test this, one group of mice received a unique and precise lipid nanoparticle injection. The mRNA inside included PUMA, the apoptotic gene, and miR-122, a microRNA that should help downregulate PUMA expression in liver cells. These mice received a stem cell transplantation seven days later. The mice in Group Two only received the stem cell transplantation.
In the following four to 16 weeks, Group Two mice fail to engraft donor cells. Comparatively, the Group One mice readily accept the transplantation—likely due to the cells having enough space to engraft.
To further validate this observation, the researchers extracted the successfully engrafted cells from Group One mice and transplanted the cells into another set of mice. Remarkably, these mice do not need pre-conditioning to engraft the donor cells. This result suggests that the initial experimental treatment paved the way for the donor cells to outcompete any remaining blood stem cells in this new set of mice.
Caveats: Possible Toxic Effects
Although the nanoparticle system can accurately target CD117 in hematopoeitic stem cells, there is a chance for the nanoparticles to impact unintended cells. One method to prevent this off-target toxicity is to integrate microRNA binding sites into the mRNA, such as miR-122. This can limit the expression of the delivered mRNA to specific cell types. Here, miR-122 prevents liver cell depletion, but more experimentation will be needed to refine this effect in other organs.
The lipid nanoparticles could also accidentally target healthy, CD117-carrying hematopoeitic stem cells. Introducing inducible suicide genes in the synthetic mRNA may help mitigate this unwanted effect. The genes would activate with a trigger (ex: administering a small molecule drug) and instruct the lipid nanoparticle to self-destruct, thus curbing off-target effects.
Future Implications
This study addresses major toxicity concerns for prospective stem cell transplant patients. The lipid nanoparticles in these mouse models accurately and safely deliver apoptotic genes to blood stem cells, thus depleting their numbers. An additional benefit is that mRNA-carrying nanoparticles can deliver more than just pro-apoptotic genes. The lipid nanoparticles described in upcoming installations carry different synthetic mRNAs to produce striking results. To conclude, mRNA technology may one day replace dangerous, one-trick-pony conditioning regimes such as chemotherapy. However, further testing will be necessary to confirm this method’s clinical feasibility.