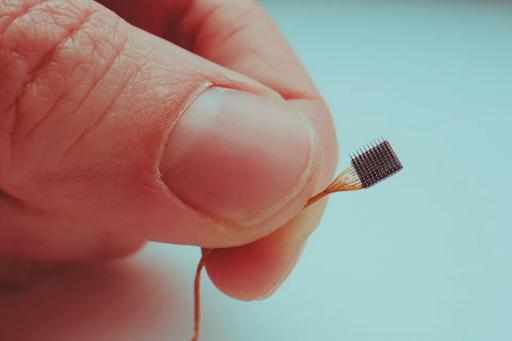
Brain-machine interface implant electrodes
This story is part of a series on the current progression in Regenerative Medicine. This piece discusses advances in brain-machine interfaces.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
Brain-machine interfaces face significant hurdles, despite scientific advances in the field. In previous months, I have discussed a number of advances in brain-machine interfaces in regenerative medicine that could improve the lives of thousands, if not millions, of people living with a range of ailments. However, we remain years away from the widespread adoption of brain-machine interfaces. A recent article in Stat News discussed the hurdles facing brain-machine interface commercialization. Here I will analyze these hurdles and discuss the future of brain-machine interfaces in regenerative medicine.
From a medical perspective, brain-machine interfaces are the next step in regenerative medicine. Those suffering from paralysis, limb loss, or other motor dysfunctions can regain the mobility they have lost. For instance, I recently discussed a decoder that takes thoughts from a patient and translates those thoughts into words. Other advances could restore partial sight to the blind, motor function to paraplegics, and so on.
From a commercial perspective, however, some have concerns about the widespread viability of brain-machine interfaces. In the Stat News article, author Lizzy Lawrence lists some issues that could become prevalent as companies attempt to bring these advances to the general public.
The first major concern for brain-machine interfaces is the development and production costs of brain chip technologies. Private equity firms have invested heavily into companies such as Elon Musk’s Neuralink, spending billions of dollars on developing brain chip-driven interfaces that have yet to be approved for human testing.
Chip production, at the time of writing, is incredibly limited. Costs for chip production fluctuate between several hundred to several thousand dollars per unit. Costs remain high because materials for production are expensive, and the product is not yet available to the public.
In an interview with The Verge, a materials scientist, Dr. Christopher Bettinger, discusses the limitations of current brain-machine interface materials. He notes that the most common material today, silicon, is too rigid to facilitate long-lasting connections with brain tissue. Small movements in the chip can elicit inflammation or even scarring, impacting the lifespan of the device.
Using silicon and other polymers introduces difficulties not only for long-term maintenance but also for initial implantation. Bettinger says polymers must be molded and implanted in “unusual or boutique ways” to yield proper results.
Other materials are in progress, including Bettinger’s own polymer film, which is much thinner and more flexible than previous materials, which hopefully will bring down production costs for the chips in the near future. It is crucial for the success of brain-machine interfaces to have low-cost, high-efficiency methods of brain chip production, something the industry currently lacks.
Another concern is that the market for these devices is not large enough to sustain their expensive research and development. While there are roughly 42.5 million people in the United and a further 1.3 billion people worldwide living with a significant disability, the vast majority will not be able to afford a costly intervention, despite the proposed upside of improving their condition.
In 2022, a study by the Commonwealth Fund found that 43% of working-age adults were inadequately insured, meaning they were uninsured, underinsured, or in an insurance gap. The median household income is just $67,000.
While the medical advances in brain-machine interfaces are incredible, they are also expensive. The NIH claims that the initial cost for a brain-machine interface is between $5,000 and $10,000, with required ongoing technical support for the duration of use.
At least in the early years, brain-machine interfaces will be a medical intervention for the wealthy, and there is a concern that there may not be enough market demand to keep the leading companies afloat.
Lawrence references Second Sight, which sold retinal implants in the late 2010s. The company reached an agreement with Medicare to receive $150,000 per device implanted, but even this unprecedented windfall could not cover their significant infrastructure costs, as the company only reached 350 patients before halting operations.
Finally, there are medical concerns as well. With invasive surgeries required to implant chips with electrodes directly onto the brain, there are risks of brain damage, hemorrhaging, infections, and so on. Chips will also require regular upkeep to maintain effective function, requiring semiregular surgical procedures, which introduces risk.
While these challenges do not need to be addressed with haste, they will become more apparent as brain-machine interface technologies advance. We are not decades away from commercializing these devices, but years.
In my view, the potential upside of improving the lives of thousands, if not millions, should outweigh financial viability concerns over the devices. Everyone has a right to live a healthy life, and we should strive to ensure that right by emboldening those who develop these technologies. As research and development continue, brain-machine interfaces will become more advanced and less expensive, calming some of the concerns we have today.
To read more of this series, please visit www.williamhaseltine.com