Gosline is in his mid-40s, healthy, and fit. This wasn’t supposed to happen.
But it did, and it’s part of a worldwide trend. An array of cancers — colorectal chief among them — are striking people younger than 50 at higher rates than in previous decades, prompting new screening guidelines, new research, and growing concern.
Why is this happening?
That’s “the very hard question that none of us really know the answer to,” said Timothy Rebbeck, professor of cancer prevention at the Harvard T.H. Chan School Of Public Health.
Theories abound, although none has firm data behind it.
But experts share a belief that the rise in cancer among younger adults may be driven by changes in the way many of us have lived our lives over the past half century.
“People born in 1990 have over double the risk of getting colon cancer compared to those born in 1950. And quadruple the risk of getting rectal cancer,” said Dr. Kimmie Ng, director of the Young-Onset Colorectal Cancer Center at the Dana-Farber Cancer Institute.
That means that at age 35, someone born in 1990 will face quadruple the risk of rectal cancer and double the risk of colon cancer when compared with the risk faced by a 35-year-old who was born in 1950.
Whether it’s sitting all day, consuming cured meats and sugar-sweetened drinks, taking antibiotics, or staying up late with the lights on, these practices — their effects probably interacting — seem to have had a profound impact on the internal workings of our bodies, disrupting metabolism and boosting inflammation.
Starting early in life and accumulating over the years, these behaviors can promote cancer in some people, in ways that are little understood.
A flurry of research is underway to get to the bottom of it. But one thing is clear: Genes alone are not to blame.
Despite the overall increase in cancer, the incidence of hereditary cancers likely hasn’t changed, said Dr. Andrew T. Chan, a gastroenterologist and chief of the Clinical and Translational Epidemiology Unit at Massachusetts General Hospital.
“The underlying genetic risk profile for cancer hasn’t shifted over the last several decades,” Chan said. “This points to the idea that cancer is very much also a disease of environment and lifestyle — it’s not just about your genes.”
But genes may play a role in how any individual responds to a given risk factor.
“The hypothesis is that there are susceptible people out there who are now being exposed to more risk factors or exposed to those risk factors earlier,” Rebbeck said.
Cancer remains about 20 times more common among older people than among the young. But doctors are concerned about the upward trend, as they increasingly diagnose malignancies once infrequently seen in anyone under 50.
Colorectal cancer has increased in people younger than 50 by about 2 percent a year since the 1990s. The rise is seen “in both men and women and in all races and ethnicities and around the world,” said Ng, of Dana-Farber.
Breast cancer has also shown an accelerating increase among women under 50, rising only slightly from 2000 to 2015 but increasing by 2 percent a year from 2015 to 2019.
Recognizing these trends, in 2021 the US Preventive Services Task Force lowered the recommended age to begin colon cancer screening to 45, and this year it proposed that breast cancer screening start at age 40 instead of 50.
Still, the trend isn’t limited to these two cancers. An analysis of data from 44 countries, published last fall, showed that more than a dozen cancers have increased among people under 50. The most common cancer types trending upward were breast, colorectal, uterine, kidney, and thyroid cancers among women, and colorectal, kidney, liver, prostate, and thyroid cancers among men (although increased screening may account for the last two). But other cancers have also increased in many countries, said Dr. Tomotaka Ugai, an instructor at Harvard Medical School who led the research.
Pancreatic cancer, an especially deadly disease with only a 10 percent survival rate, is also increasing among young people, said Dr. Brian M. Wolpin, director of the Gastrointestinal Cancer Center at Dana-Farber. According to National Cancer Institute data, pancreatic cancer among men younger than 50 increased 6.5 percent a year from 2017 to 2019; the yearly increase among women was 2.4 percent from 2000 to 2019. Pancreatic cancer is expected to strike 64,000 Americans this year, compared with 300,000 breast cancer cases and 153,000 colorectal cancers.
The behaviors that predispose people to pancreatic cancer at any age seem to be magnified in the young, Wolpin said. For example, while smoking will increase the risk of pancreatic cancer for anyone, that effect is especially strong at younger ages.
Obesity, as defined by BMI or body-mass index, remains the prime suspect in the search for the cause of early-onset cancers, especially for colorectal cancer, for several reasons. One is circumstantial: The average BMI rose in parallel with early-onset colorectal cancer, increasing at the same rate over the same time period.
The habits that can cause people to gain weight — lack of exercise, poor diet, sweetened beverages — also boost cancer risk.
But even independent of those factors, experts say, carrying excess fat by itself can fuel cancer by affecting hormones, insulin, and metabolism.
“The actions of obesity are to change hormones, to change inflammation,” Rebbeck said. “So obesity itself can be an outward sign of things going on in your body that are associated with cancer.”
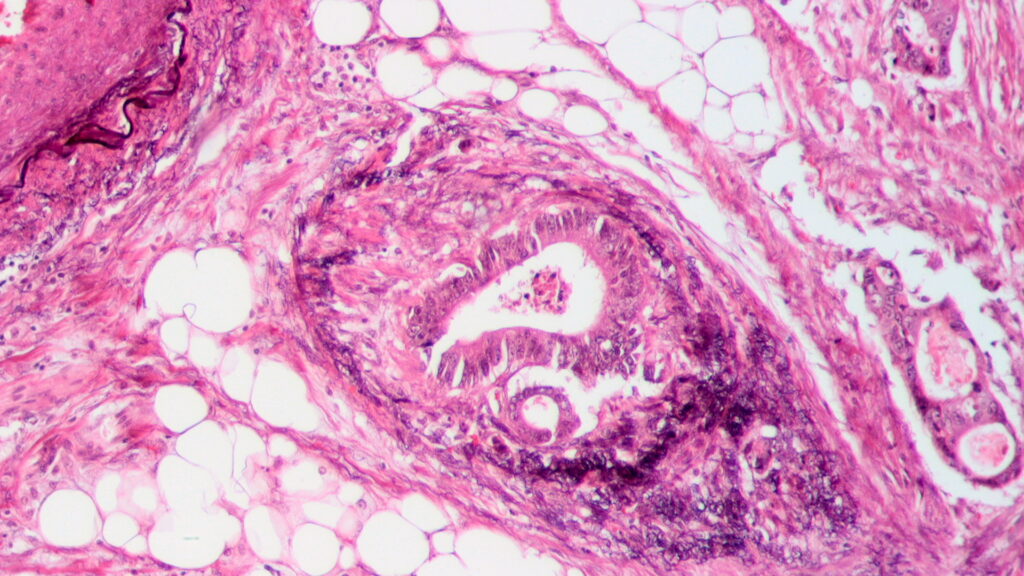
Obesity may induce “a low grade inflammatory environment within the lining of the colon,” said Dr. Joel B. Mason, professor of medicine and nutrition at Tufts University. “And by doing so, it provokes certain changes in the cells that line the colon and that ultimately can lead precancerous and cancerous tumors to develop.”
Localities identified as economically disadvantaged bear a disproportionate burden of early-onset colorectal cancer and those same areas also have higher rates of obesity, Mason said. “Is it merely the lifestyle that’s associated with being economically or socially disadvantaged? Or is it specifically obesity itself? Or is it both these factors?”
Still, says Ng, not every study supports the notion that obesity leads to cancer in the young.
“And anecdotally, I can just tell you that so many of my young patients that we see are perfectly fit,” she added. “They’re marathon runners, they have healthy diets, they are not obese. And so it does go beyond just obesity.”
Chris Gosline is one of her patients.
When Ng told Gosline that he had stage 4 colorectal cancer a year ago, he was stunned. “I’m not overweight. I’ve been running my whole life. I eat well, I don’t smoke, I don’t drink heavily. I don’t do drugs of any sort,” he said. “You feel like you’re following all the rules , doing right by your body, then out of nowhere….”
Plus, going back generations his family has no history of cancer.
Gosline started a chemotherapy regimen that involves eight weeks of infusions followed by a four-week break. He’s also switched to a low-carbohydrate diet that limits sugar and red meat, and includes healthy oils like avocado.
A year after his diagnosis, Gosline, who is 45 and lives with his wife and son in Manchester-by-the-Sea, says he’s responding well to the chemo. The tumors in his colon and liver are not visible on scans. But no one has spoken of remission or told him he could stop the chemo. “No one knows exactly what the future holds,” he said.
Gosline has been able to continue working through treatment. He owns a company that operates solar farm battery storage units.
“I haven’t slowed down at all,” he said. “I keep pushing through.” When he’s undergoing chemo, he continues the infusions at home, carrying around a bag of medicine for 48 hours.
When an infusion is done, he goes running. “I’ll start a run and feel terrible. When I’m done with the run it feels very helpful. … I’m in the best shape of my life right now, very fit.” He runs four to five miles every other day with weekly longer runs.
“There’s a lot of us out there, come to find out,” Gosline said. “People living a healthy profile. Then, out of nowhere it’s, boom, you have cancer. … There’s something going on out there, some variable.”
Ng is among those investigating what those variables may be. “We do think that it may be other changes in the environment,” Ng said. “Is it increasing antibiotic use? Is it components of these ultra processed foods that have emerged with modern lifestyles, that is changing the microbiome?”
The community of microbes that live in the intestines, known as the gut microbiome, is critical to health, and plays a role in digestion and in stimulating the immune system. The microbiome can be disrupted by chronic stress, a poor diet, and antibiotics, among other things, and such disruption could be a factor in promoting cancer.
The role of obesity gets complicated when it comes to breast cancer. Women who were overweight as children have a lower risk of cancer throughout their lifetime, while after menopause obesity increases the risk, said Heather Eliassen, professor of nutrition and epidemiology at the Harvard T. H. Chan School of Public Health. After menopause when the ovaries stop producing estrogen, Eliassen said, fat tissue converts other hormones into estrogen, which fuels the growth of cancer cells.
Some of the increase in breast cancer results from changes in reproductive choices, especially having a first child later in life, as many women do these days, she added.
During pregnancy, breast tissue changes in ways that can protect against the mutations that lead to cancer — provided the pregnancy happens early in life. But when decades elapse between the start of menstruation and the first pregnancy, women accumulate damage to the DNA in their breast tissue. Then, pregnancy “can fuel the growth of cells that may be harboring mutations,” Eliassen said, leaving women at higher risk of breast cancer for five or 10 years after a pregnancy.
So women who bear their first child in their mid- to late 30s or early 40s are at greater risk than women who never become pregnant. And women who never have a pregnancy are at greater risk than those who have their first child in their 20s.
To make matters worse, Eliassen said, the type of breast tumors that form before menopause tend to be harder to treat and more aggressive.
This is true of many early-onset cancers, including in the colon: They tend to be more aggressive. That may be because they’re detected later — most young people don’t screen for cancer or suspect it as the cause of symptoms.
But there are also hints that early-onset cancers are biologically different from cancers later in life.
Chan, the Harvard epidemiologist, said his young adult patients who undergo colonoscopies to check on a gastrointestinal complaint often find they already have polyps, a precursor to colon cancer. “We’re finding polyps at 25 or 30 years old,” he said. “It’s clear that there is something different happening even before someone turns 25.”
Strangely, colon cancer tumors in young people typically form on the left side of the colon and in the rectum, Ng said, while no such pattern is seen in the old. No one knows why. And young people with metastatic colon cancer, even if they are more fit and receiving more intensive therapy, have survival rates no better than older people, according to recent research at Dana-Farber.
“The very youngest patients do seem to have a biologically different disease,” Ng said.
But experts caution that none of this bad news should leave people feeling helpless. While the roots of cancer may form early in life, Chan said, “I don’t think anyone should think there’s a point of no return.”
We already know a lot about the clear risks to health, Rebbeck said. Ample data show that certain things are bad for you — ultraprocessed foods, cigarettes, alcohol, sugar-sweetened beverages, lack of physical activity, inadequate sleep.
“Sleep, diet, exercise — those things are actionable,” Rebbeck said. “And so they are very important because you may be able to do something about them.”
Experts see reason to stay hopeful. Treatment for both colon cancer and breast cancer has improved and survival rates keep going up.
And there is lots of promising research underway. Dana-Farber’s Beyond CRC Project is enrolling early-onset colon cancer patients in a study that will gather detailed information on lifestyle and diet, analyze tumors, and collect blood and stool samples.
The National Cancer Institute and Cancer Research UK have listed early-onset cancer as one of the “grand challenges” for researchers and will award $25 million next year to a winning team.
“It is encouraging that so much attention is being paid to the early-onset cancer issue,” Rebbeck said. “There is scientific progress being made, and I hope we will have answers.”